Spotlight Series
Stay updated with insights from Adial’s executives on the latest company news and key developments in addiction research.
View All Spotlight SeriesUncorking the truth: Why women’s alcohol use is rising and what we’re missing in treatment
November 19, 2025
A conversation with Dr. Robertson on the trend of rising rates of alcoholism among women
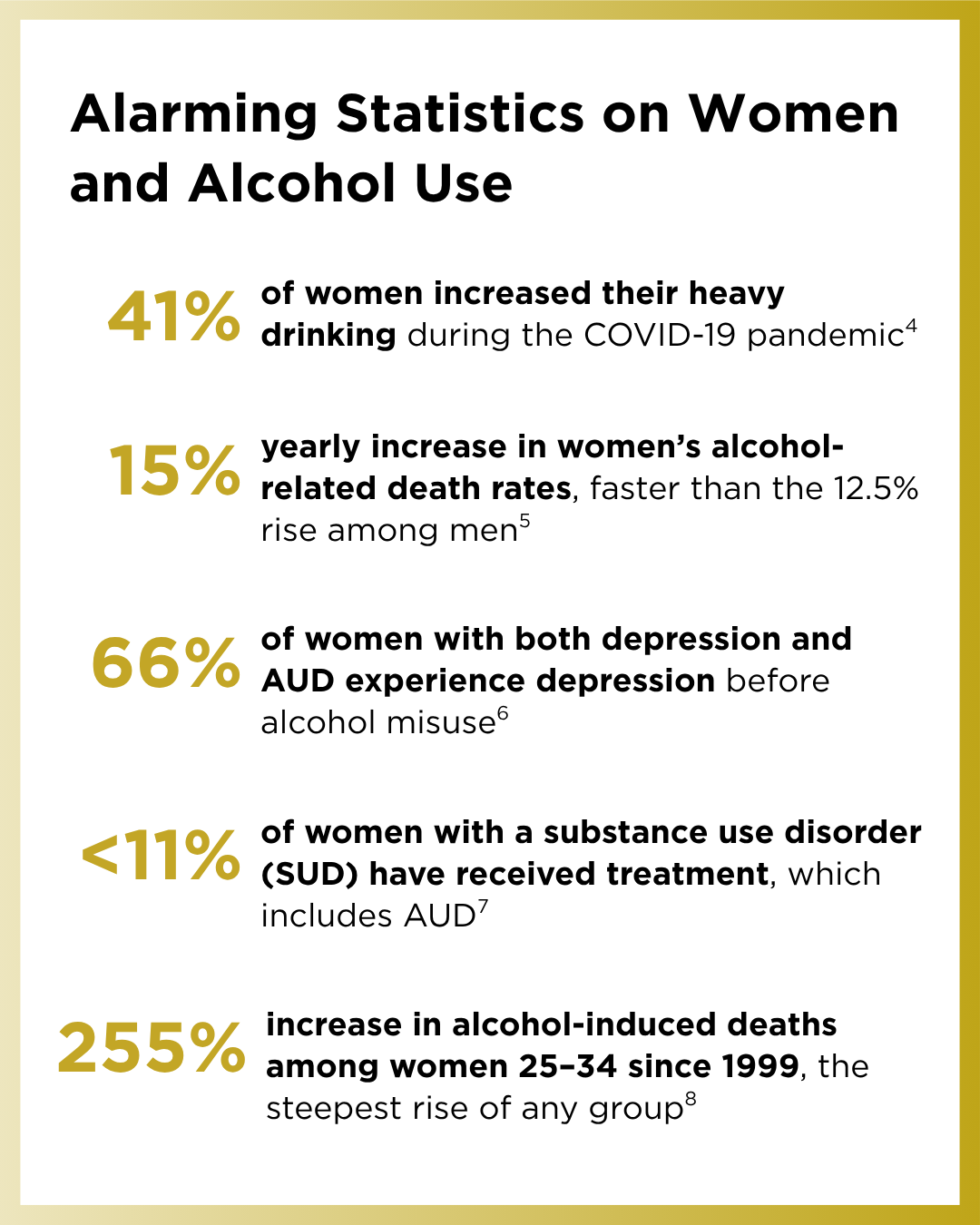
Over the past several decades, alcohol use among women has climbed to unprecedented levels. In fact, women have nearly closed the historical gap in drinking rates between genders. Yet this equalizing of consumption comes at a steep cost: Women suffer disproportionately severe health consequences from alcohol. Recent public health data show alarming trends. For instance, alcohol-related deaths among U.S. women jumped 35% between 2016 and 2021 compared to 27% among men[1]. Likewise, alcohol-related hospitalizations increased 69% among women over a 15-year period versus 43% among men[2]. These numbers underscore an urgent and growing crisis in Alcohol Use Disorder (AUD) among women.
We sat down with Adial Pharmaceuticals’ Acting Chief Medical Officer, Brigitte Robertson, MD, to discuss the link between AUD and women, why it’s becoming a more urgent issue, and the steps we as a society can take to improve care for women.
Why has Alcohol Use Disorder (AUD) among women accelerated, and what makes this an important issue?
Dr. Robertson: Over the past two decades, the relationship between alcohol and women has undergone a quiet but significant transformation. Initially, alcohol in small amounts was seen as a way to enhance social events, easing tension lowering anxiety and self-consciousness, making it easier to connect and engage with others. Today, alcohol has evolved into a lifestyle symbol, particularly for women.
Social trends like the ‘mommy-wine culture,’ wellness-themed cocktails, and heavy influencer marketing have not just helped normalize drinking, but have glamorized drinking in women. Media has played a key role in driving this shift by framing alcohol as a tool for empowerment, self-care, and social belonging, across every modality, from reality TV and lifestyle blogs to influencer-driven branding, that links drinking to wellness and identity.
This cultural messaging has blurred the line between occasional context-based use and habitual reliance. For many women, alcohol has inadvertently become a patterned coping response to chronic stressors such as professional demands, caregiving responsibilities, and emotional overload- not because it solves these pressures, but because it’s legal, widely accessible, socially reinforced, and rarely questioned.
One area of growing concern is the risk of progression. Once a woman meets even a single high-risk DSM-5 criterion (e.g., such as symptoms of withdrawal or continued drinking despite harm), the likelihood of progressing from mild to severe AUD rises sharply to ~60–70%. Compounding this is the risk-severity paradox. Women tend to experience more
These trends converge into a critical inflection point: more women are drinking heavily, progressing more rapidly to severe alcohol use disorder (AUD), and yet remain largely severe health consequences at lower consumption, for instance the risk of premature-mortality rises at ~1.8 drinks/day in women versus ~3.2 in men[3].
Perhaps most troubling is that the majority of women who meet diagnostic criteria for AUD remain untreated, a reflection of how often these cases are overlooked in clinical practice.
These trends converge into a critical inflection point: more women are drinking heavily, progressing more rapidly to severe alcohol use disorder (AUD), and yet remain largely invisible within traditional treatment frameworks. The data are stark, rising death rates, underdiagnosis, and treatment gaps, underscoring a systemic failure to recognize gender-specific risk trajectories. Women now represent a substantial and growing share of the estimated 30 million Americans with AUD[9], yet most existing interventions were designed around male-centric models of addiction. Addressing this crisis requires more than awareness; it demands a reimagining of care, one that integrates biological sensitivity, psychiatric comorbidity, and the social realities that shape women’s drinking patterns.
What differences make women more susceptible to alcohol-related harm?
Dr. Robertson: Women experience more harm at lower levels of alcohol consumption due to a constellation of biological factors. Metabolically, they have lower gastric enzyme activity and less body water, leading to higher blood alcohol concentrations per drink compared to men.
Hormonal differences also play a role. Fluctuations in estrogen and progesterone change how alcohol feels and how quickly craving and relapse risk build. Alcohol can also raise estrogen by tying up the liver enzymes that normally clear it, creating a feedback loop. Meanwhile, acetaldehyde, the toxic byproduct of alcohol, damages cells; paired with estrogen-driven cell growth, that increases the risk of hormone-sensitive cancers, including ER-positive breast cancer (about 70% of breast cancers are ER-positive)[10].
Neurobiologically, women show stronger reactivity in stress related neurocircuitry, including the amygdala, part of the brain’s primal threat-response system often referred to as the “lizard brain.” This system governs fast, non-executive reactions to danger and acts as the brain’s rapid-response alarm. Women tend to show stronger amygdala responses to stress and to alcohol cues. Over time, this heightened reactivity also raises vulnerability to anxiety and depression, creating a cycle where stress triggers drinking, drinking strengthens the cues, and the next stress hits harder, increasing vulnerability to anxiety, depression, and progression to alcohol use disorder.
How does AD04’s mechanism align with women’s stress-related drinking behaviors?
Dr. Robertson: For many women, alcohol use is tightly bound to stress and cue-driven craving, so the right therapy has to fit real biology and real life. At Adial Pharmaceuticals, we are advancing the development of AD04 (ondansetron) so patients can regain control without forcing day-one abstinence, aligning clinical goals with how many women want to engage in care.
AD04 blocks 5-HT3A and 5-HT3AB, the receptors that modulate serotonergic circuits tightly linked to stress, craving, and reinforcement, as well as affecting some peripheral receptors in the gut and that have to do with inflammation. By engaging these pathways and brainstem/autonomic circuits relevant to withdrawal and autonomic dysfunction, AD04 targets key drivers of stress-related drinking that are especially salient for women.
Our goal has always been to meet patients where they are and help them move toward healthier patterns safely and sustainably. Many women want to regain control of their drinking, but the idea of quitting “cold turkey” immediately is not always desirable given the social aspects of drinking and the perceived stigma surrounding alcohol use disorder.
What parallels do you see between psychiatric treatment models and women’s AUD care?
Dr. Robertson: Psychiatry is moving away from treating the “average patient” and focusing effort on matching care to biology, subtype, and life context. AUD in women needs the same shift. It’s a biologically rooted, neurobiological illness; for many women, stress- and cue-driven drinking, not just reward and reinforcement, drives risk, so care must support self-control, and fit patients’ real lives.
Many women want to regain control before abstinence, so we support a non-abstinence, harm-reduction approach. In short, personalized by biology and subtype, meet patients where they are, and build pathways women can actually use and sustain.
AUD carries a lot of stigma, especially for women. What is Adial Pharmaceuticals’ position to ensure patients get compassionate, patient-centric support?
Dr. Robertson: We’re not “reframing” AUD so much as recognizing and managing it as a medical condition with clear biological underpinnings. Like any chronic illness, it develops through identifiable mechanisms, responds to targeted treatment, and deserves the same clinical attention and public understanding as conditions like hypertension or obesity. The science is clear; now our responsibility is to ensure that both clinical care and public mindset reflect that reality, with the same diagnostic precision, therapeutic rigor, and informed understanding we apply to conditions like hypertension or obesity. Stigma keeps women out of care. Many women fear being judged or labeled “unfit,” worry about losing autonomy, and don’t want to be seen walking into a clinic. Women are underrepresented in programs, even though they often arrive with more severe psychological and medical issues. Those barriers are compounded when anxiety or depression masks AUD, or vice versa.
Many women don’t seek care because they fear being perceived as unstable, unfit, or incapable, concerns that can threaten their sense of autonomy, privacy, and social standing. Seeking treatment may carry social or professional consequences that should not exist in a modern healthcare system. Yet these perceived risks continue to deter women from seeking care, contributing to their underrepresentation in treatment programs, even though they often present with more complex medical and psychiatric profiles. These barriers are further compounded when co-occurring conditions like anxiety or depression obscure the diagnosis of Alcohol Use Disorder, or when alcohol use itself masks deeper clinical needs.
Our stance is practical: Meet women where they are and make entry safe, in judgment-free environments, virtual and in-person, so privacy, safety, and autonomy concerns don’t keep them out of care. Education about sex-specific drivers, trauma, and social context is essential, and care should be flexible and reduce barriers in general and for the individual.
Why is AD04 well-suited for a precision, harm-reduction approach to women’s AUD?
Dr. Robertson: AD04 addresses a large and growing unmet need. Women represent an increasing share of AUD cases, but treatments often haven’t been designed around women’s biology and life context. The faster-rising harm in women (in terms of deaths, hospital visits, etc.) creates an urgent need for a new solution.
AUD remains a huge public health and economic burden by costing the U.S. on the order of $250 billion each year, and much of that burden lies in sub-optimally treated or untreated patients[11]. We aim to deliver better outcomes for a population that has been underserved, which in turn can translate to meaningful savings for healthcare systems.
We foresee AD04 being at the forefront of a new generation of AUD therapeutics: one that is genotype-guided and centered on harm reduction. In sum, AD04 is uniquely positioned because it marries scientific precision with real-world patient preferences. It offers a path to recovery that is realistic and compassionate, a combination that has been missing in the alcohol treatment field and one that we believe can profoundly reduce the burden of AUD in women.
[1] U.S. Centers for Disease Control and Prevention, Morbidity and Mortality Weekly Report, “Deaths from Excessive Alcohol Use — United States, 2016–2021” 2024
[2] National Institute on Alcohol Abuse and Alcoholism, “NIAAA Surveillance Report #112,” 2018
[3] National Institute on Alcohol Abuse and Alcoholism (NIAAA), Screening and Behavioral Counseling Interventions to Reduce Unhealthy Alcohol Use in Adolescents and Adults: An Updated Systematic Review for the U.S. Preventive Services Task Force, 2018
[4] RAND, “Alcohol Consumption Rises Sharply During Pandemic Shutdown; Heavy Drinking by Women Rises 41%,” 2020
[5] Harvard Women’s Health Watch, “Alcohol-related deaths rising faster among women,” 2023
[6] Journal of Studies on Alcohol, “The co-occurrence of alcoholism with other psychiatric disorders in the general population and its impact on treatment,” 2015
[7] Penn State Social Science Research Institute, “Women less likely to seek substance use treatment due to stigma, logistics,” 2023
[8] PLOS Global Public Health Journal, “Alcohol-induced deaths in the United States across age, race, gender, geography, and the COVID-19 pandemic,” 2025
[9] SAMHSA, 2022 National Survey on Drug Use and Health (NSDUH)
[10] National Institute of Health: National Cancer Institute, Alcohol and Cancer Risk, 2025
[11] National Institute on Alcohol Abuse and Alcoholism (NIAAA)